A Guide to Risk Management in Healthcare

Risk management advisors have the responsibility of creating a plan that includes all practices and procedures and meets the demands of all interested parties. This means that as the advisor, you’ll need to review the needs of each of the organization’s stakeholders — including the leadership, staff, patients, visitors, and community you serve.
While no single plan applies to all types of practice environments, using the steps below can help you create a plan unique to your specific needs and the risks specific to your organization and practice. For example, if your facility is a college health clinic, your risks will be different from those of a dental office.
Remember: This structure is just a sample recommendation. You must design a plan that’s tailored specifically to your organization and its needs. That may require additional topics and categories not listed here, or the revision or removal of items we included. Here are the steps to take to create a risk management plan and process for your organization.
The plan should begin with a list of these elements:
You will want to consult with your organization’s leadership and/or legal department for guidance as you develop and finalize your plan. You may also want to consider scheduling recurring reviews of the final plan once it’s complete (e.g., at least once a year).
The strategies you’ll use to identify risks should depend largely on the focus and scope of your organization. Methods used to identify risk can be as simple as interviewing your staff to compile a list of past events that occurred or as complex as implementing diagrammatic identification techniques, like a Fault Tree Analysis or Ishikawa and Fishbone’s Cause and Effect.
The goal of this step is not only to determine as many possible and actual risks as possible, but also to include the policies, procedures, general practices, and organizational structure of the physical environment so that risks are identified and planned for.
Once you determine what your risks are, you’ll then want to assess the probability of an adverse event actually happening. Analyzing the probability of each risk is done both qualitatively and quantitatively.
From these assessments, you’ll be able to decide where to prioritize your risk prevention efforts, starting first with the high qualitative risks that also have high quantitative impacts.
Once you’ve analyzed each established risk in Step 3, plan your responses to the possible risk in the processes below. It’s also helpful to delegate each risk to a particular staff person to take precautionary (mitigation) and reactionary (contingency) measures. That way, if the adverse event does happen, your team knows who owns the risk and how to respond.
Once a risk occurs, you have to allow for reporting, controlling, and monitoring the events that follow. Ongoing assessment of these planned responses is required, as well as continuously evaluating all risk. This includes:
We created an example of a healthcare risk management plan using the steps and structure shown above. For the sake of easy reading, we’ve broken up the plan into two sections: Step 1 will be in bullets, while Steps 2-5 will be in a table. Ideally, this format will allow you to view each risk prevention step and reaction process in an organized layout.
Here’s what an example of what Step 1 could look like:
And here’s an example of what Steps 2-5 could look like:
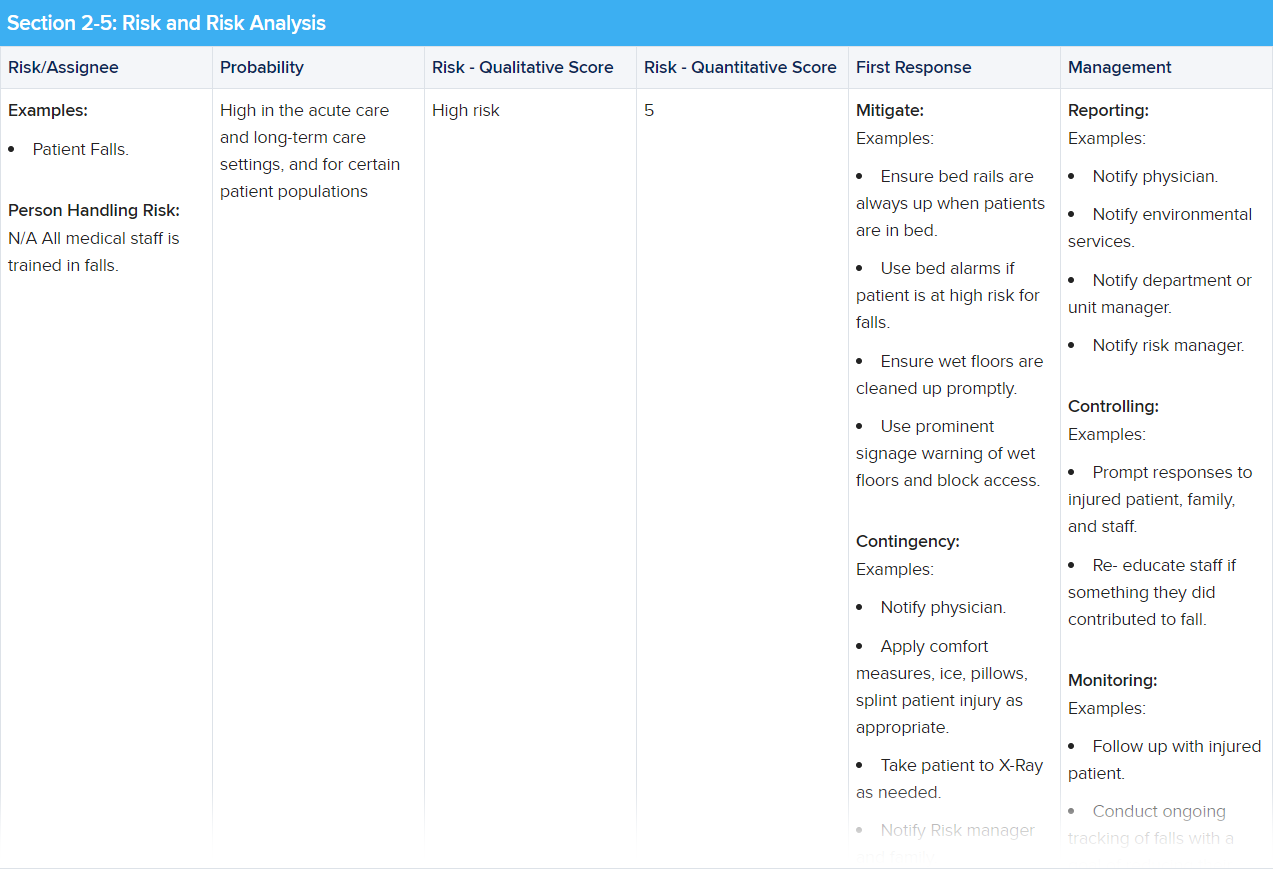
One example of how you can format a healthcare risk management plan.
Image courtesy of iStock.com/tzahiV
Last updated on Aug 25, 2021.
Originally published on Aug 14, 2018.
Previous Section:
What Is Risk Management in Healthcare?More:
The views expressed in this article are those of the author and do not necessarily reflect those of Berxi™ or Berkshire Hathaway Specialty Insurance Company. This article (subject to change without notice) is for informational purposes only, and does not constitute professional advice. Click here to read our full disclaimer
The product descriptions provided here are only brief summaries and may be changed without notice. The full coverage terms and details, including limitations and exclusions, are contained in the insurance policy. If you have questions about coverage available under our plans, please review the policy or contact us at 833-242-3794 or support@berxi.com. “20% savings” is based on industry pricing averages.
Berxi™ is a part of Berkshire Hathaway Specialty Insurance (BHSI). Insurance products are distributed through Berkshire Hathaway Global Insurance Services, California License # 0K09397. BHSI is part of Berkshire Hathaway’s National Indemnity group of insurance companies, consisting of National Indemnity and its affiliates, which hold financial strength ratings of A++ from AM Best and AA+ from Standard & Poor’s. The rating scales can be found at www.ambest.com and www.standardandpoors.com, respectively.
No warranty, guarantee, or representation, either expressed or implied, is made as to the correctness, accuracy, completeness, adequacy, or sufficiency of any representation or information. Any opinions expressed herein are subject to change without notice.
The information on this web site is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment, and does not purport to establish a standard of care under any circumstances. All content, including text, graphics, images and information, contained on or available through this web site is for general information purposes only based upon the information available at the time of presentation, and does not constitute medical, legal, regulatory, compliance, financial, professional, or any other advice.
BHSI makes no representation and assumes no responsibility or liability for the accuracy of information contained on or available through this web site, and such information is subject to change without notice. You are encouraged to consider and confirm any information obtained from or through this web site with other sources, and review all information regarding any medical condition or treatment with your physician or medical care provider. NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY SEEKING MEDICAL TREATMENT BECAUSE OF SOMETHING THAT YOU HAVE READ ON OR ACCESSED THROUGH THIS WEB SITE.
BHSI is not a medical organization, and does not recommend, endorse or make any representation about the efficacy, appropriateness or suitability of any specific tests, products, procedures, treatments, services, opinions, health care providers or other information contained on or available through this web site. BHSI IS NOT RESPONSIBLE FOR, AND EXPRESSLY DISCLAIMS ALL LIABILITY FOR, ANY ADVICE, COURSE OF TREATMENT, DIAGNOSIS OR ANY OTHER SERVICES OR PRODUCTS THAT YOU OBTAIN AFTER REVIEWING THIS WEB SITE.
Click to collapse disclamerWant Berxi articles delivered straight to your inbox? Sign up for our monthly newsletter below!
"*" indicates required fields